Wisdom Tooth Discomfort Is Common — Infection Requires Closer Attention
Wisdom teeth often cause discomfort, especially when they are erupting, partially erupted, or difficult to clean. Not all wisdom tooth pain means infection. However, infection is one of the most common reasons wisdom tooth pain becomes urgent.
The difference is not always how much something hurts, but how symptoms behave over time.
Why Wisdom Teeth Commonly Cause Pain
Wisdom teeth erupt later than other teeth and often lack adequate space. Discomfort can occur due to:
- Pressure as the tooth pushes against gum tissue
- Inflammation around a partially erupted tooth
- Food and bacteria trapped beneath a gum flap
- Contact or crowding against neighboring teeth
This type of pain is usually localized and may fluctuate rather than steadily worsen.
Signs of Wisdom Tooth Pain Without Infection
Wisdom tooth pain is more likely to be non-infectious when it is:
- Mild to moderate and localized
- Triggered mainly by chewing or pressure
- Intermittent rather than constant
- Not associated with swelling, drainage, or systemic symptoms
This does not mean evaluation is unnecessary, but stable symptoms may not require emergency care.
What a Wisdom Tooth Infection Is
A wisdom tooth infection develops when bacteria multiply in the tissue around the tooth or spread into deeper structures. This is more likely when a wisdom tooth is:
- Partially erupted
- Difficult to clean effectively
- Repeatedly trapping food and bacteria under the gum
Once infection develops, symptoms typically change in pattern, not just intensity.
Signs Wisdom Tooth Pain May Be an Infection
Wisdom tooth pain is more likely related to infection when one or more of the following occur:
Increasing or Constant Pain
Pain that worsens over time, becomes constant, or disrupts sleep suggests progression rather than irritation.
Swelling Around the Tooth or Jaw
Swelling of the gums, jaw, cheek, or face—especially if it feels firm, warm, or continues to expand—is a common sign of infection.
Redness, Drainage, or Persistent Bad Taste
Red, inflamed gum tissue, pus, or a bad taste that does not resolve may indicate active infection.
Difficulty Opening the Mouth
Jaw stiffness or limited opening can occur when infection spreads into surrounding tissues.
Fever or Feeling Unwell
Fever, fatigue, or a general sense of illness suggests the body is responding systemically.
Why Wisdom Tooth Infections Can Progress Quickly
The location of wisdom teeth makes infections harder to drain and easier to spread. Without treatment, infection may extend into:
- Adjacent teeth
- Jawbone
- Soft tissues of the face and neck
For this reason, wisdom tooth infections are a common cause of urgent dental visits.
When to Seek Emergency Dental Care
Urgent evaluation is recommended when wisdom tooth pain is accompanied by:
- Rapidly increasing or spreading swelling
- Difficulty opening the mouth or swallowing
- Fever or worsening facial pain
- Drainage or signs of spreading infection
You can learn more about urgent warning signs and next steps on our Emergency Dentistry page.
How Dentists Distinguish Pain From Infection
During an evaluation, the dentist may:
- Examine the surrounding gum tissue
- Check for swelling, drainage, or tenderness
- Take X-rays to assess the tooth and surrounding bone
- Determine whether the tooth can be monitored or should be removed
Treatment decisions are based on risk and predictability, not pain level alone.
Why Early Evaluation Matters
Wisdom tooth pain that is evaluated early may be managed with:
- Monitoring and hygiene guidance
- Medication when appropriate
- Planned extraction under controlled conditions
Waiting until infection is advanced can narrow options and increase urgency.
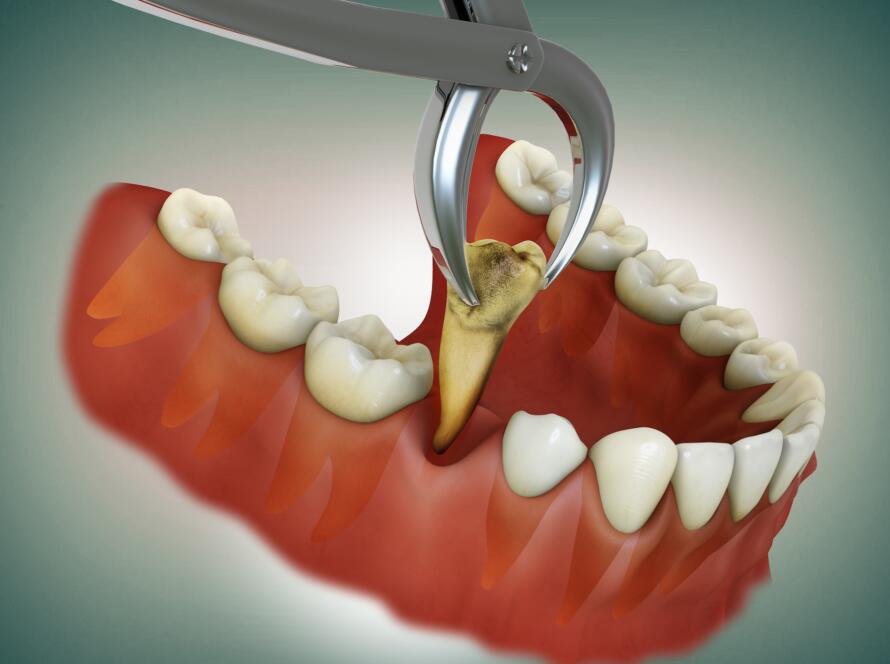
A Note on Wisdom Tooth Removal
Not every painful wisdom tooth needs to be removed. However, when infection risk is high or symptoms recur, extraction is often the most predictable long-term solution.
You can learn more about wisdom tooth removal, recovery, and treatment options on our Extractions & Wisdom Teeth page.